The medical industry is familiar with the use of autoclaves in operating rooms and laboratory settings for sterilization. However, a recent trend in the medical device industry is to evaluate the environmental impact on the identification markings and function of reusable medical devices after repeated autoclave sterilization cycles.
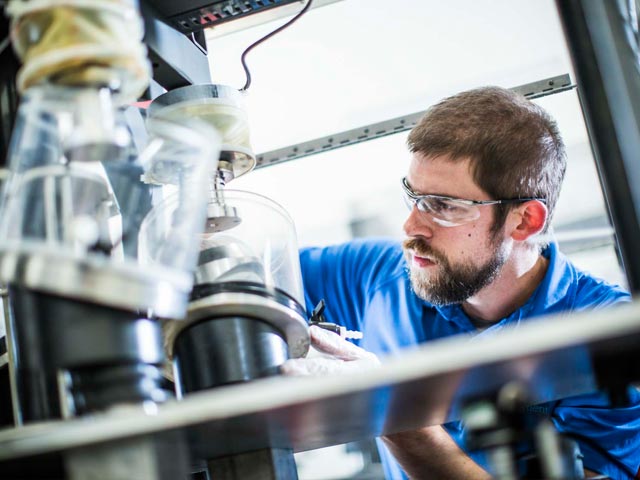
Reusable medical device validation intends to follow the standard cleaning procedures, and repeatedly cycle the parts in an autoclave to expose the instrumentation to cyclical environmental aging. Testing instruments in the environmental chamber of an autoclave compresses the overall lifetime of the instruments into a few weeks.
Reusable medical device validation evaluates instrument dimensions, functionality, and susceptibility to corrosion or chemical breakdown over time. Understanding the performance of the device or instrument can help determine the life cycle before the product needs to be removed from service.
Identification wear and discoloration
唯一的设备标识(UDI)规定要求uire that medical devices contain a unique device identifier on the device labels and packaging to trace the device from manufacture through the end of its life cycle. The Global Unique Device Identification Database (GUDID) manages device information tied to this UDI. The label needs to be marked on the device to maintain traceability and should be readable in plain text as well as machine-readable throughout its life cycle. These regulations are currently in place in the US, with Europe adding UDI requirements to align with those around the world.
With the new MDR regulation requiring all reusable medical devices to be labeled with a UDI number, repeated exposure to steam sterilization cycles has the potential to degrade or wear the identifying labels down. Reusable medical device validation with an autoclave helps determine not only the life cycle of the instrument itself but that of the required label markings as well. If a mark is worn or degrades to a point where it is no longer readable, this should effectively end the life cycle of the part unless it can be easily relabeled.
Materials degradation or performance
Materials used in reusable medical instruments such as polymers, synthetics, and metals are sensitive to moisture, heat, and pressure. These factors are known to accelerate the degradation and failure of these materials. Examples of observations that may apply to material performance are unusual deformation, cracking, odor, peeling, leaching, and residues. Not only could the material become compromised, and therefore the instrument itself, appearance can play a factor as many instrument families are color-coded for ease during surgery.
Dimensional inspection
During use and sterilization processes, instruments manufactured from plastics and resins may experience thermal and residual stresses that could alter the performance and appearance of the device. Dimensional measurements performed alongside autoclave sterilization and aging testing help track and characterize the dimensional stability of instruments before use in the field. Particular attention should be given to dimensions which may relate to the sizing of the actual implant or other critical features. Dimensional inspection is especially helpful when developing or implementing new instrument materials and understanding maximum and minimum material conditions and tolerances.
Functionality testing
For complex or multi-component instrumentation, functionality articulations should be performed and assessed throughout testing. Functionality testing simulates the use of the instrument in the field. Assessments could include rotation and engagement of threaded components, locking and unlocking mechanisms, etc. Throughout functionality testing, any changes to the instrumentation, including wear marks, laser marking changes, debris generation, or seizing, should be evaluated and documented. The minimum number of functional cycles can be determined by reviewing the number of uses in surgeries and surgeries per month. Typical acceptance criteria for functionality testing is if the device continues to function as intended at each checkpoint and at the end of testing.
In addition to typical functionality testing, testing to failure or proof testing may be performed against a control instrument to evaluate the performance of an instrument at the beginning and end of its life cycle.
Corrosion and debris generation
If a component fails functionality testing, an investigation as to the cause of failure should be performed. Wear and corrosion debris for metal materials or cracking and peeling for polymers may be cause for failure. Additional testing, such as chemical or particle analysis, may be beneficial to debris investigations. The location and amount of debris generation can drive design changes and improve future instrument performance.
Sample autoclave cycle parameters
Autoclave parameters for aging testing should be such that they simulate the sterilization process as well as compress the testing timeline. Specific chemical reactions are accelerated as temperature increases. Pre or post-autoclave soaks may be included in the autoclaving process. Care must be taken to select the cleaning solution to ensure it does not react with the material undergoing testing. Dimensional analysis and imaging may be performed throughout the life cycle testing to track life cycle progression. Using the same equipment and setups for imaging helps avoid negative light and background influence on images. Typical autoclave process and settings for life cycle testing include:
- Prewash (optional)
- Pre-vacuum (optional, dependent on equipment)
- Wrapped/unwrapped
- Temperature: 270-273°F
- Exposure time: 4-15 min
- Drying time: 30 minutes-24 hours (depending on the application and test type)
- Dwell time between cycles
Validating reusable medical instruments with Element
Simulating life cycles to evaluate materials and design performance is critical to ensuring success in the healthcare environment. Reusable medical device validation and autoclave life cycle testing may be performed on parts already in use, new parts in development, or worst-case instruments. Factors to consider when selecting samples for testing are material (metal vs. nonmetal), single components/fixed assemblies, multi-component assemblies, the complexity of devices, and overall geometry (joints, crevices/gaps, lumens, etc.). Making an initial investment to validate reusable medical instruments can result in cost and time savings when lifetime performance is understood and predicted.
Element offers a full suite of testing and validation services for single-use and reusable medical devices. For more information on how we can support your next project or request a quote,contact us today.
making certain for nearly 190 years
More from Element
sector
Medical Device
As a comprehensive testing partner, you’ll enjoy the benefit of a single supplier source for all of your testing needs, from mechanical testing and environmental simulation to EMC and wireless device testing.
Read More

services
Accelerated Aging Shelf Life Testing
Our shelf life testing can help you determine how climatic & environmental factors like humidity, temperature, and light affect the lifespan and integrity of your products.
read More

resource
乐动LOL
发现博客、文章、白皮书,webinars, and advice from our world-leading testing, inspection, and certification experts.
Read More
Subscription Center
Sign-up for free resources
Visit Element's email subscription center to receive the latest industry news, technical whitepapers, case studies, webinars, and upcoming events.
Read More




